Services
Our goal through Pain Management is reducing and eliminating chronic pain while restoring function and quality of life.
Pain Management
Treatments
Stimulation
Injections
Injections
& Kyphoplasty
Nerve Block
Ablation
Treatment
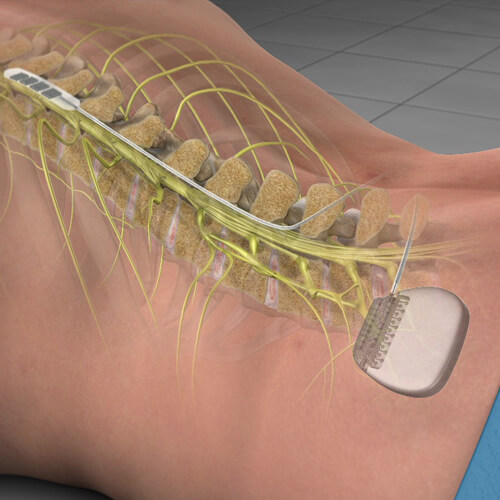
Spinal Cord Stimulation
Spinal cord stimulation may help relieve pain and improve quality of life in people with chronic (long-lasting) pain, such as low back and leg pain. Spinal cord stimulation (SCS) may help reduce and manage chronic pain that does not go away with physical therapy, pain medications, injections, or other non-surgical treatments. Advances in SCS technology have allowed people with chronic spine-related pain to reduce or eliminate their need for pain medications and return to comfortable, productive lives. SCS is best at treating neuropathic pain from a pinched or injured nerve, and is also good at treating mechanical back pain from such conditions as degenerative disc disease, radiculopathy (pain that radiates down an arm or leg), spinal stenosis (narrowing of the spinal canal), failed back surgery (pain that remains following surgery), and sciatica. In addition, SCS is useful in treating nerve pain from hernias, intercostal neuralgia (rib pain following surgery), and complex regional pain syndrome (CRPS), which is a relatively uncommon form of chronic pain. Spinal cord stimulation is used to treat chronic peripheral neuropathic pain, which is damage to nerves outside of the spinal cord (typically in the hands or feet) that is caused by an infection, trauma, surgery, diabetes, or other unknown causes. Each patient should undergo a SCS trial before the device is implanted to make sure that the pain is relieved by this treatment.
During the trial period, a temporary SCS is placed in the back for a period of 5 to 10 days. The trial allows the patient to learn how to use the system, become familiar with the way it feels, and see what degree of comfort and pain relief it provides. The SCS trial is the best prognostic guide to how much pain relief will be provided with a permanent SCS system. While you might not have complete pain relief, a greater than 50% decrease in pain with SCS is considered successful. You may be eligible for permanent placement of a spinal cord stimulator if your trial is successful.
Treatment
Joint Injections
Non-surgical procedure which delivers steroids directly into a joint, such as a knee, shoulder, or hip.
Treatment
Epidural Steroid Injection
An epidural steroid injection refers to an injection of medicine onto an area within the spinal column but outside the spinal cord. A maximum of 6 injections in a 1-year period is recommended, but the maximum allowed depends on your insurance. There is no evidence to support a series of 3 injections. The decision to have a second injection should be based on the effect of the first injection. The primary benefit of spinal injection is to provide relief of pain and disability. Spinal injections are typically well tolerated and safe with an extremely low rate of complications. The most common risks include small amounts of bleeding, headache, and facial flushing. More major complications include puncture of the dura, infection, and nerve damage. These major complications occur in less than 1% of people undergoing spine injections. People with diabetes may note a temporary elevation of their blood sugars. It is difficult to predict how long an injection will last given the many variables at play unique to each patient.
Most people can expect to receive 1.5 to 3 months of pain relief. In some cases, an injection may provide minimal or only a few days of pain relief, while other patients may see symptom improvement up to a year after receiving an injection.
Treatment
Kyphoplasty &
Vertebroplasty
Spinal compression fractures, also known as vertebral compression fractures (or VCFs), may be treated with surgery. Balloon kyphoplasty, and vertebroplasty are two minimally invasive treatments for thoracic (mid-back) and lumbar (low back) spinal compression fractures. During kyphoplasty (also called balloon kyphoplasty), a thin tube is inserted into the collapsed vertebra (spinal bone). Attached to the tube is a small balloon that, when inflated, moves the broken bone and creates an open space. The balloon is removed, and the space is filled with thick, liquid bone cement. Balloon kyphoplasty can help relieve back pain and stabilize the vertebral compression spinal fracture. In addition, kyphoplasty may also restore fracture-related lost vertebral height, thus reducing or preventing spinal deformity.
During vertebroplasty, bone cement is injected into the collapsed vertebral body. The bone cement rapidly sets, hardens and stabilizes the spinal fracture. Vertebroplasty can help to relieve pain and may strengthen other vertebral bodies at risk for fracture. However with vertebroplasty, no balloon is used to possibly restore vertebral body height.
Treatment
Medial Branch Nerve Block
Treatment
Radiofrequency Ablation
Outpatient treatment involving pulsed radio waves that temporarily disable nerves from transmitting pain signals to the brain.
Radiofrequency ablation (RFA) is a minimally invasive treatment performed on an outpatient basis to treat painful neck or back facet joints or sacroiliac joint pain after medial branch blocks have been performed and shown to be successful. The treatment involves use of pulsed radio waves produced at a high frequency that temporarily stun/disable nerves from transmitting pain signals to the brain. It can take upwards of two to four weeks in most cases for the ablated nerves to stop sending pain signals. Pain relief may last 3-6 months or longer. While radiofrequency ablation disables nerves from conducting pain, the solution is not permanent as the nerves will grow back, but the procedure can be repeated if necessary.
The benefits of this treatment include longer lasting pain relief, it is minimally invasive, has low complications, and patients have quick recovery.
Pain Management
Conditions
Sciatica is not a disorder itself but is a general term used to describe leg pain that occurs when nerve roots in the low back become compressed (pinched), irritated, or inflamed, often from a herniated or bulging disc, or other narrowing of the spinal canal. Sciatica may be accompanied by numbness/tingling and muscle weakness of the leg. Pain is the hallmark sciatica symptom.
Although sciatica symptoms may be felt anywhere along the sciatic nerve, classic sciatica radiates from the low back into the butt, and down the leg to below the knee. Less commonly, sciatica pain may be felt starting in the buttocks or hip area and radiates down the leg. Sciatica pain is often described as electric, burning, or sharp. The nerve pain can vary from mild to excruciating and can worsen when you bend down, twist your spine, or cough. Although you have two sciatic nerves (one on each side of your body), sciatica symptoms typically only occur on one side of the body.
Common causes of sciatica are herniated discs, degenerative disc disease, bone spurs, spondylolisthesis, vertebral fracture, and piriformis syndrome. Other conditions like sacroiliac joint dysfunction and iliotibial band syndrome can mimic the symptoms of sciatica, but are not truly caused by sciatic nerve impingement or irritation. The cause of sciatic is diagnosed by medical history, physical exam, and imaging studies. Non-surgical treatment includes physical therapy, medications, epidural steroid injections, and other interventional procedures.
Early disc degeneration may not cause severe pain or other symptoms, but when the degeneration becomes advanced low back pain may occur. Typically, discogenic pain is associated with activities that increase the pressure within the intervertebral disc.
These activities may include bending, sitting, standing, coughing, or sneezing. Individuals can have discogenic pain and also have leg pain from a nerve being pinched. A disc can develop tears resulting in the development of this pain. Degenerative discs can be seen with a MRI. If one or more spinal discs are suspected as the pain source, a provocative discogram or discography may be performed to aid in diagnosis.
During this sterile procedure, the suspect discs are injected with a contrast dye to make each disc visible under fluoroscopy. Provocative discography helps the doctor to see the shape and size of the intervertebral disc. The injection of the contrast dye alters the pressure within the disc and may reproduce the patient’s pain pattern. This helps to isolate a particular disc as a pain generator. Non-surgical treatments may include medications, physical therapy, spinal injections, and epidural steroid injections.
Degenerative disc disease (DDD) is typically associated with aging. As you age, your discs, like other joints in the body, can degenerate (break down) and become problematic: That’s a natural part of growing older as your body deals with years of strain, overuse, and maybe even misuse. It is the normal wear and tear that occurs as part of the aging process of your spine. However, DDD can occur in young people as well. Degenerative disc disease involves the intervertebral discs. Those are the shock absorbing cushions between the bones that make up the spine. They are the part of your back that support weight while helping to allow motion.
As you age, the discs can lose flexibility, elasticity, and shock absorbing characteristics. They also become thinner as they dehydrate. When all that happens, the discs change from a supple state that allows fluid movement to a stiff and rigid state that restricts your movement and causes neck and/or back pain. It is interesting to note that although 80% of adults will experience back pain, only 1% to 2% will need lumbar spine surgery. Non-surgical treatments may include medications, physical therapy, spinal injections, and epidural steroid injections.
Also known as a slipped disc or ruptured disc, a herniated disc is a relatively common condition that can occur anywhere along the spine, but most often affects the lower back or neck region. A herniated disc develops when one of the cushion-like pads between the vertebrae moves out of position and presses on adjacent nerves. Herniated discs are typically caused by overuse injuries or trauma to the spine; however, disc conditions can also develop as a result of the normal aging process. Herniated discs are most commonly caused by wear and tear, repetitive movements, lifting incorrectly, trauma, and obesity.
Symptoms usually include a pain in the back or leg, numbness, tingling, burning, muscle spasms or weakness, and possibly loss of bowel or bladder control. A herniated disc in the lower back can heal within six months of onset, as the size of herniation shrinks with time via resorption. Surgery may be needed if bowel or bladder control is lost, or if medication, physical therapy and other treatments fail. Non-surgical treatments may include medications, physical therapy, spinal injections, and epidural steroid injections.
Piriformis syndrome occurs when the piriformis muscle, located deep in the buttock, compresses the sciatic nerve. The piriformis muscle originates at the sacrum and attaches to a bone at the outermost part of the hip. The piriformis helps turn your hip outward and bringing your thigh outward to one side while your hip is bent, such as when raising your knee and bringing your leg out when getting out of a car seat. It also offers stability while walking, running and standing.
Usually, the sciatic nerve passes directly underneath the piriformis before continuing down the back of the thigh. But for some, the sciatic nerve passes directly through the piriformis predisposing such people to piriformis syndrome. While piriformis syndrome doesn’t always present exactly the same way, common symptoms include pain in the buttocks that’s worse when sitting, especially with the legs crossed in a figure of four position. Maintaining that position for long periods can cause pain that radiates down one leg.
Other symptoms may include pain with sitting, standing or walking for short periods of time, pain when standing up from seated or squatting, and pain that improves with movement. Non-surgical treatments may include medications, physical therapy, epidural steroid injections, or muscular trigger point injections.
A joint connects 2 or more bones in your body. Your back and neck have joints at each level to allow motion known as facet joints or facets. When these joints become painful, a patient can experience increased stiffness and difficulty or pain with onset of activity, changing positions, bending backwards, or raising up from a forward bent position. The effects of aging, wear and tear, and/or traumatic injury such as a fall or motor vehicle accident can damage the facet joints and lead to back pain known as facet joint syndrome.
Treatment of this condition is usually a combination of nonsurgical treatments including anti-inflammatory medication, core strengthening exercises, and stretching. If these conservative treatments have not been enough to manage a patients pain complaints, other options include interventional procedures such as medial branch joint blocks and radiofrequency ablation.
Sacroiliac (SI) joint dysfunction is a common cause of low back pain. This condition can make daily activities, such as sitting, standing, walking, and even sleeping difficult. In a study of low back pain, sacroiliac joint dysfunction was found in upwards of 30% of patients. Due to the joint being close to other parts of the body that can commonly cause pain, it’s not unusual for SI joint dysfunction to be mistaken for other causes of low back pain, such as a herniated or bulging disc.
Causes of SI dysfunction include arthritis, pregnancy, trauma, or infection. Symptoms of SI dysfunction include pain with activity, climbing stairs, pain aggravated by standing or walking for long periods, and pain that improves with lying flat.
Treatments include medication, physical therapy, epidural injections, facet joint and sacroiliac joint injections or nerve blocks.
After spine surgery, you expect your back or neck problem to be resolved. But, sometimes, that doesn’t happen. Whether immediately or months after your procedure, pain and other symptoms may return—a phenomenon known as failed back surgery (FBS). Also called failed back surgery syndrome (FBSS) and post-laminectomy syndrome. Having failed back surgery doesn’t suggest that you or your surgeon have failed. What it means is that your surgeon’s expected outcome of pain relief and increased function did not happen.
To be diagnosed with FBS, your physician must be able to link your current issue to your previous spinal surgery. It is believed that this condition occurs following back surgery between 10-40% of patients. The success with recurrent surgeries has also been shown to decrease as well, with a success of 50% after the first repeat surgery and 15% after the third. That is why repeat surgery isn’t always the answer. Non-surgical treatment options include physical therapy, medications, epidural steroid injections, facet joint injections, and spinal cord stimulation.
You might think of arthritis as something you get in your hands, shoulders, knees or hips, but it can happen in your spine as well. It’s called spondylosis, also known as spinal osteoarthritis. “Arthritis” is really an umbrella term for painful joints. Osteoarthritis is caused by cartilage breakdown; cartilage provides a cushion between the bones of the joints.
Healthy cartilage allows bones to glide over one another and acts as a shock absorber during physical movement. In osteoarthritis, the cartilage breaks down and wears away. This causes the bones under the cartilage to rub together, causing pain, swelling, and loss of joint motion. Risk factors for osteoarthritis include increased age, female gender, joint injuries, obesity, and diseases that affect cartilage. Possible symptoms of arthritis include swelling or tenderness of the joint especially with weather changes, reduction in flexibility, stiffness with onset of activity, bony nodules around the joint, grinding of the joint with use, and pain with usage of the joint.
Possible treatment includes medications, physical therapy, facet joint injections for the back, and steroid or lubricating injections for the extremities.
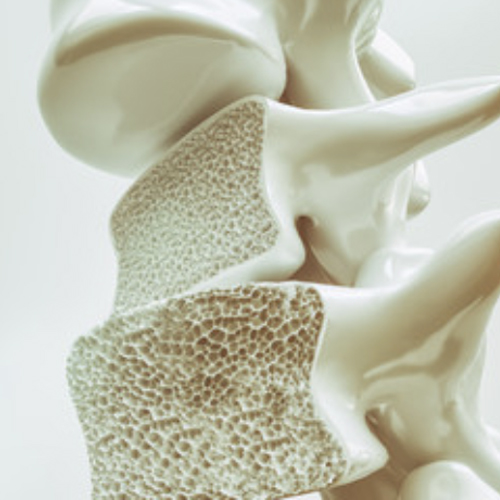
Osteoporosis is commonly called the “fragile bone disease.” It is due to loss of bone density caused by a deficiency in such bone-building nutrients as calcium, vitamin D, magnesium and other vitamins and minerals. One of the most common results of osteoporosis is vertebral compression fractures. In people with advanced osteoporosis, compression fractures can occur as the result of coughing, sneezing, bending, carrying heavy loads, or experiencing a fall.
Compression fractures occur when the vertebrae collapse, decreasing their size by 15-20% or more. This compression causes chronic back pain, loss of height, deformity, and in severe cases neurological symptoms such as numbness, tingling, or weakness. If there are multiple compression fractures along the vertebral column, difficulty walking and a loss of balance is common. Compression fractures are often diagnosed only after a person seeks medical attention either for pain relief or after a fall. However, many compression fractures go undiagnosed and their symptoms are attributed to being an inevitable part of aging.
Traditional treatment for compression fractures include pain medications, bed rest, bracing or, in very severe cases, surgery. Today there are two minimally invasive treatments for compression fractures called vertebroplasty and kyphoplasty.
Osteoporosis
Stimulation
Injections
Injections
& Kyphoplasty
Nerve Block
Symptoms and Causes
Bone Health Osteoporosis
Sed ut perspiciatis unde omnis iste natus error sit voluptatem accusantium doloremque laudantium, totam rem aperiam, eaque ipsa quae ab illo inventore veritatis et quasi architecto beatae vitae dicta sunt explicabo. Nemo enim ipsam voluptatem quia voluptas sit.
Our Approach
Osteoporosis is commonly called the “fragile bone disease.” It is due to loss of bone density caused by a deficiency in such bone-building nutrients as calcium, vitamin D, magnesium and other vitamins and minerals. One of the most common results of osteoporosis is vertebral compression fractures. In people with advanced osteoporosis, compression fractures can occur as the result of coughing, sneezing, bending, carrying heavy loads, or experiencing a fall. Compression fractures occur when the vertebrae collapse, decreasing their size by 15-20% or more. This compression causes chronic back pain, loss of height, deformity, and in severe cases neurological symptoms such as numbness, tingling, or weakness. If there are multiple compression fractures along the vertebral column, difficulty walking and a loss of balance is common. Compression fractures are often diagnosed only after a person seeks medical attention either for pain relief or after a fall. However, many compression fractures go undiagnosed and their symptoms are attributed to being an inevitable part of aging. Traditional treatment for compression fractures include pain medications, bed rest, bracing or, in very severe cases, surgery. Today there are two minimally invasive treatments for compression fractures called vertebroplasty and kyphoplasty.
Symptoms and Causes
Spinal Chord
Stimulation
Sed ut perspiciatis unde omnis iste natus error sit voluptatem accusantium doloremque laudantium, totam rem aperiam, eaque ipsa quae ab illo inventore veritatis et quasi architecto beatae vitae dicta sunt explicabo. Nemo enim ipsam voluptatem quia voluptas sit.
Our Approach
Sed ut perspiciatis unde omnis iste natus error sit voluptatem accusantium doloremque laudantium, totam rem aperiam, eaque ipsa quae ab illo inventore veritatis et quasi architecto beatae vitae dicta sunt explicabo. Nemo enim ipsam voluptatem quia voluptas sit aspernatur aut odit aut fugit, sed quia consequuntur
Symptoms and Causes
Joint Injections
Sed ut perspiciatis unde omnis iste natus error sit voluptatem accusantium doloremque laudantium, totam rem aperiam, eaque ipsa quae ab illo inventore veritatis et quasi architecto beatae vitae dicta sunt explicabo. Nemo enim ipsam voluptatem quia voluptas sit.
Our Approach
Sed ut perspiciatis unde omnis iste natus error sit voluptatem accusantium doloremque laudantium, totam rem aperiam, eaque ipsa quae ab illo inventore veritatis et quasi architecto beatae vitae dicta sunt explicabo. Nemo enim ipsam voluptatem quia voluptas sit aspernatur aut odit aut fugit, sed quia consequuntur
Start living pain free. Contact us today!
Joint
Injections
Sed ut perspiciatis unde omnis iste natus error sit voluptatem accusantium doloremque laudantium totam rem.
Symptoms and Causes
Facet Injections
Sed ut perspiciatis unde omnis iste natus error sit voluptatem accusantium doloremque laudantium, totam rem aperiam, eaque ipsa quae ab illo inventore veritatis et quasi architecto beatae vitae dicta sunt explicabo. Nemo enim ipsam voluptatem quia voluptas sit.
Our Approach
Sed ut perspiciatis unde omnis iste natus error sit voluptatem accusantium doloremque laudantium, totam rem aperiam, eaque ipsa quae ab illo inventore veritatis et quasi architecto beatae vitae dicta sunt explicabo. Nemo enim ipsam voluptatem quia voluptas sit aspernatur aut odit aut fugit, sed quia consequuntur
Start living pain free. Contact us today!
Joint
Injections
Sed ut perspiciatis unde omnis iste natus error sit voluptatem accusantium doloremque laudantium totam rem.
Symptoms and Causes
Vertebroplasty
& Kyphoplasty
Sed ut perspiciatis unde omnis iste natus error sit voluptatem accusantium doloremque laudantium, totam rem aperiam, eaque ipsa quae ab illo inventore veritatis et quasi architecto beatae vitae dicta sunt explicabo. Nemo enim ipsam voluptatem quia voluptas sit.
Our Approach
Sed ut perspiciatis unde omnis iste natus error sit voluptatem accusantium doloremque laudantium, totam rem aperiam, eaque ipsa quae ab illo inventore veritatis et quasi architecto beatae vitae dicta sunt explicabo. Nemo enim ipsam voluptatem quia voluptas sit aspernatur aut odit aut fugit, sed quia consequuntur
Start living pain free. Contact us today!
Joint
Injections
Sed ut perspiciatis unde omnis iste natus error sit voluptatem accusantium doloremque laudantium totam rem.
Symptoms and Causes
Occipital Nerve Block
Sed ut perspiciatis unde omnis iste natus error sit voluptatem accusantium doloremque laudantium, totam rem aperiam, eaque ipsa quae ab illo inventore veritatis et quasi architecto beatae vitae dicta sunt explicabo. Nemo enim ipsam voluptatem quia voluptas sit.
Our Approach
Sed ut perspiciatis unde omnis iste natus error sit voluptatem accusantium doloremque laudantium, totam rem aperiam, eaque ipsa quae ab illo inventore veritatis et quasi architecto beatae vitae dicta sunt explicabo. Nemo enim ipsam voluptatem quia voluptas sit aspernatur aut odit aut fugit, sed quia consequuntur
Start living pain free. Contact us today!
Joint
Injections
Sed ut perspiciatis unde omnis iste natus error sit voluptatem accusantium doloremque laudantium totam rem.
Treatment Process
How Does it Work?
Step 1
Schedule an appointment
Step 2
Let's find the best solution for you
Dr. Boeckman and his team of specialists will work with you to develop an interventional pain management plan to provide relief and an improved quality of life.